It’s time to understand your spine and make a plan
Eliminate your pain With Scoliosis Solution™: spine analysis, on-demand Scoliosis Realignment Therapy™, and a supportive community of scoliosis experts.

30-Day Money Back Guarantee
Has Scoliosis caused you pain and discomfort every day for years?

You're too old to make progress

What you've tried before hasn't worked

The healthcare system is working against you

You're in too much pain to exercise

You're feeling lost and hopeless

You can't find anyone near you who can help
You’re not alone. 65+ million adults are affected by Scoliosis, yet countless athletes, blue and white color professionals, and seniors have reduced or eliminated their pain, restored their function, and reduced their visual asymmetry with Scoliosis Solution™. Your solution is here and could have you living a pain-free life in as little as 2 months.

30-Day Money Back Guarantee
It’s time to understand your spine and make a plan

1. Get Access
2. Submit Your X-rays or photos

3. Implement Your Personalized Plan
Get Access To
Scoliosis Solution™
$39.99 / month

30-Day Money Back Guarantee
What You’ll Achieve With Scoliosis Solution™

Understand the root cause of your pain

Know how to realign your body without surgery

Meet others going through it

An approach and plan to live without pain

30-Day Money Back Guarantee
Heyling is pain free!
“All the knowledge and exercises have given me my life back, I’m pretty much pain-free all the time now.”

Allyson finally gets relief
“Your program has improved my strength, mobility, and flexibility, but it has also given me an overall understanding of how to work with my curves and function on a day-to-day basis. I’m grateful to you for giving me a better my life!”
Get Access To
Scoliosis Solution™
$39.99 / month

30-Day Money Back Guarantee
Your subscription gets you access to:

Spine analysis

Personalized Plan through spine analysis, recommendations, and office hours

On Demand Scoliosis Exercise Courses including Scolio-Pilates and Scoliosis Safe Yoga (Scoliosis Realignment Therapy™).

Member exclusive community office hours w/ experts

Downloadable Guides and E-Books about nutrition and daily hacks living with Scoliosis

Get Access To
Scoliosis Solution™
$39.99 / month

30-Day Money Back Guarantee
Try Scoliosis Solution's Chronic Pain Course For Free
Learn the secrets of easing your chronic pain caused by Scoliosis for free. This is just one of the many courses and lessons available in the Scoliosis Solution that can bring you life-changing results.
Meet Your Guides
Our doctor team from Stanford, Mayo, Duke, Johns Hopkins, and our scoliosis exercise practitioners across the world have worked with thousands of people with scoliosis. In that time, we’ve seen the heartbreaking realities of countless adults who unnecessarily suffered for decades. That’s why we teamed up with several of the top and mission-driven orthopedic physicians in to develop Scoliosis Solution™.

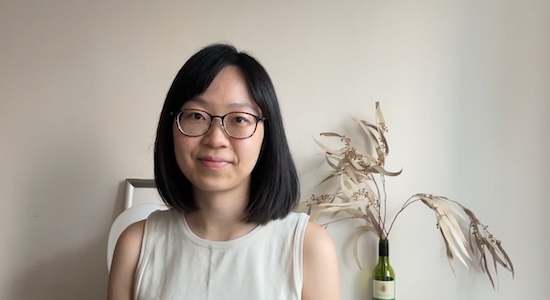
Karena Thek
Founder of Scolio-Pilates® the largest scoliosis training company in North America. Over the past 10 years, her 40+ practitioners have helped over 100,000 scoliosis patients eliminate their pain.
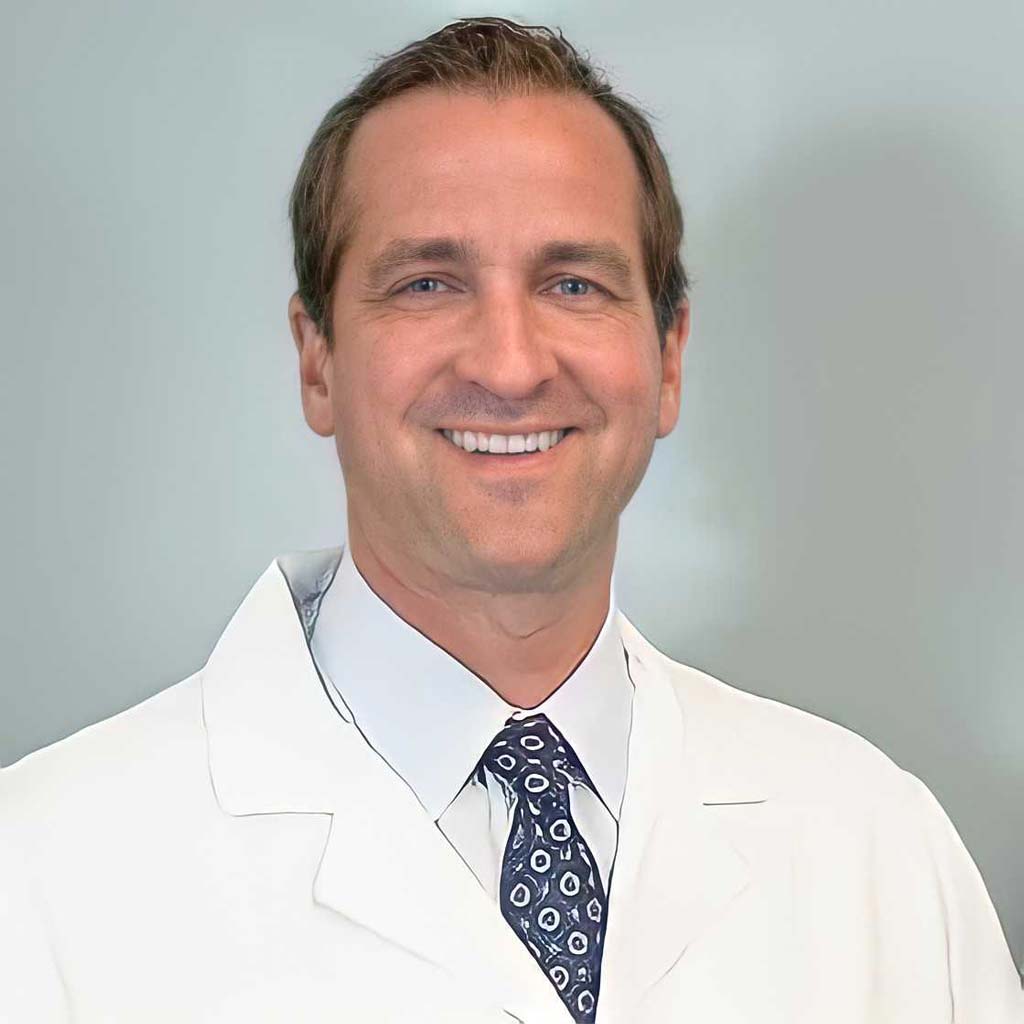
Dr. Michael Gardner, MD
Co-founder of the National Scoliosis Clinic and Professor, Orthopaedic Surgery, Stanford University. Has personally worked with over 20,000 patients and performed over 8,000 orthopedic surgeries.

30-Day Money Back Guarantee
Kevon Is Pain Free!
“After dealing with pain for 23 years, I haven’t had any pain in my neck and shoulders after my first week of Scoliosis Solution. I sent in my x rays, understood my spine, and got a personalized plan!”
Scoliosis Solution™ FAQs
I've had a spinal fusion surgery, is this program appropriate for me?
The Scoliosis Solution programs are usually helpful for people with fused spines. A fused spine can continue to change above and below where the fusion has occurred. Our program attempts to relieve the pressure on the points above and below and address any additional curvature that may be happening.
I have Arthritis, Osteoporosis, Kyphosis, or other musculoskeletal conditions, is this program appropriate for me?
For any individual we always encourage seeking approval from your care team to determine if exercise is safe and appropriate for you. For more info about specific conditions, please see below:
- Osteoporosis: Our program adheres to safe movement practices for those with low bone density, a condition that varies in severity. We focus on avoiding excessive stress on the spine. Specifically, for osteoporosis, we avoid extreme bending, side-bending, and twisting movements. These actions are also avoided in our Scoliosis Solution program, as they are not recommended for scoliosis.
- Arthritis: Movement is recommended for people with osteoarthritis; there are no contraindications to exercise for this condition.
- Kyphosis: This is not a kyphosis specific program. When people have kyphosis combined with scoliosis, it’s usually helpful.
Can I cancel at any time or is there a certain amount of time you have to sign up for?
Yes, members can cancel at any time, there is no minimum or maximum amount of time that people have to participate in the program
What equipment do I need to participate in the exercise?
You can perform the Scoliosis Solution program whenever and wherever is most convenient for you. Here’s all you’ll need:
- Your computer, smartphone, or tablet, with internet access.
- An open area. You’ll need a few feet of empty space to move in. You may want to use a yoga mat or blanket for floor exercises.
- Washclothes and 2 Beach towels (depending on video)
- if you can but not necessary: resistance band, squishy ball and wedges.
What ages is this program for?
Almost any age can participate in this program, Karena has worked with clients who were in their 90’s who saw benefits. In general, this program is appropriate for those who are older than 10 years old.
Is the membership HSA eligible?
If you don’t have an HSA card, you can pay with your credit card or other card, and request a reimbursement from your HSA following your HSA provider’s available methods.

30-Day Money Back Guarantee
Medical Advisors

John Vorhies, MD
Pediatric Spine Surgeon
Stanford University
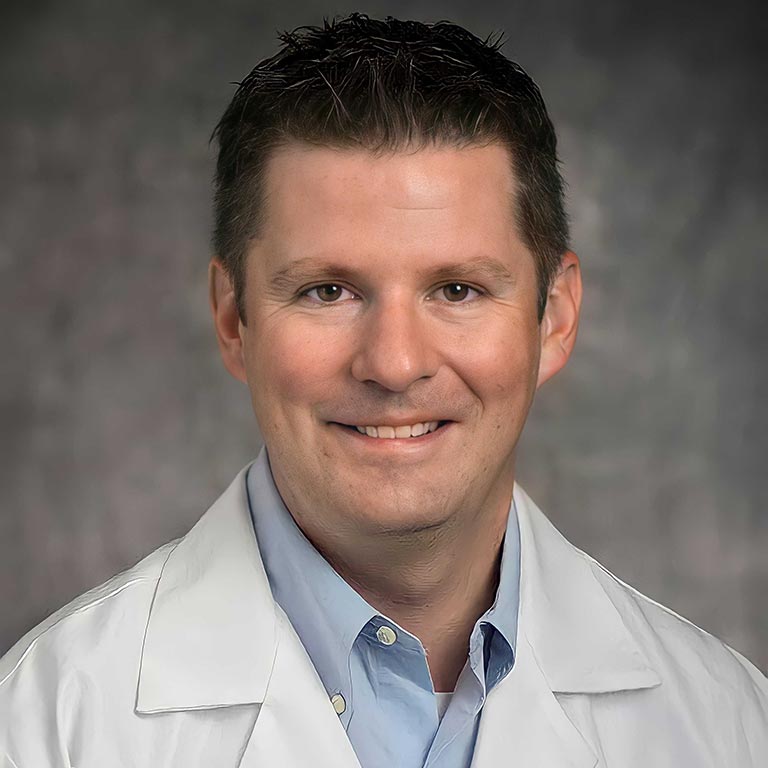
Michael Glotzbecker, MD
Case Western Reserve University
Amer Samdani, MD
Philadelphia Shriners

Todd Milbrandt, MD
Mayo Clinic

Craig Louer, MD
Vanderbilt University

Amit Jain, MD
Johns Hopkins University School of Medicine
Get Access To
Scoliosis Solution™
$39.99 / month
